Does musculoskeletal discomfort at work predict future musculoskeletal pain? |

Does musculoskeletal discomfort at work predict future musculoskeletal pain?
Authors:
Heleen H. Hamberg-van Reenen abc; Allard J. van der Beek ab; Birgitte M. Blatter ac; Maarten P. van der Grinten c; Willem van Mechelen ab;Paulien M. Bongers ac
DOI: 10.1080/00140130701743433
Publication Frequency:
12 issues per year
To cite this Article: Reenen, Heleen H. Hamberg-van , van der Beek, Allard J. , Blatter, Birgitte M. , van der Grinten, Maarten P. , van Mechelen, Willem andBongers, Paulien M. (2008) 'Does musculoskeletal discomfort at work predict future musculoskeletal pain?', Ergonomics, 51:5, 637 - 648 AbstractThe objective of this prospective cohort study
was to evaluate if peak or cumulative musculoskeletal discomfort may
predict future low-back, neck or shoulder pain among symptom-free
workers. At baseline, discomfort per body region was rated on a
10-point scale six times during a working day. Questionnaires on pain
were sent out three times during follow-up. Peak discomfort was defined
as a discomfort level of 2 at least once during a day; cumulative
discomfort was defined as the sum of discomfort during the day.
Reference workers reported a rating of zero at each measurement. Peak
discomfort was a predictor of low-back pain (relative risk (RR) 1.79),
neck pain (RR 2.56), right or left shoulder pain (RR 1.91 and 1.90).
Cumulative discomfort predicted neck pain (RR 2.35), right or left
shoulder pain (RR 2.45 and 1.64). These results suggest that both peak
and cumulative discomfort could predict future musculoskeletal pain.
1. IntroductionMusculoskeletal pain is common among the working population. Both the demands at work and the capacity of the worker to perform work-related activities may play a role in the development of this pain, which has been stated in the load-tolerance model (Panel on Musculoskeletal Disorders and the Workplace 2001). In previous studies, high exposure to work-related physical factors (Hoogendoorn et al. 2000, Ariëns et al. 2001), low physical capacity (Hamberg-van Reenen et al. 2006a) and an imbalance between those two factors (Hamberg-van Reenen et al. 2006b) were found to be associated with musculoskeletal pain in the long term. However, these associations were not consistently found for all work-related factors and physical capacity parameters. In the short term, an imbalance between work-related physical factors and physical capacity may lead to musculoskeletal discomfort in and around active and passive structures (i.e. muscles, tendons and joints). Musculoskeletal discomfort can become manifest as tension, fatigue, soreness, heat or tremor (van der Grinten and Smitt 1992). Perceived musculoskeletal discomfort is generally used as a subjective indicator of short-term effects. In the case of insufficient recovery, short-term effects may end as more permanent effects, that is, musculoskeletal pain (Winkel and Mathiassen 1994, van der Beek and Frings-Dresen 1998). In many studies reporting on short-term musculoskeletal discomfort as an indication of the effect of an ergonomic intervention, the authors assume that musculoskeletal discomfort can predict musculoskeletal pain in the long term (Genaidy et al. 1995, Galinsky et al. 2000, Mclean et al. 2001, Fenety and Walker 2002, Babski-Reeves et al. 2005, Wahlstrom 2005). However, to the authors' knowledge, this relationship has been investigated in only one longitudinal study (Werner et al. 2005a,b), in which a relationship was found between baseline neck or shoulder discomfort and future upper extremity tendonitis. In the present study, it was hypothesised that musculoskeletal discomfort may predict future musculoskeletal pain, with two potential aetiological mechanisms on the basis of that relationship. The first hypothesis was that at least one moment of discomfort during a working day, as an indicator of peak exposure to work-related physical factors, is a risk factor for future musculoskeletal pain. The second hypothesis was that cumulative discomfort during a working day, as an indicator of cumulative exposure to work-related physical factors, is a risk factor for future musculoskeletal pain. The objective of this prospective cohort study was to evaluate the two hypotheses that peak levels of musculoskeletal discomfort and/or cumulative discomfort may predict future musculoskeletal pain among symptom-free workers. 2 Methods2.1 Study designThe longitudinal Study on Musculoskeletal disorders, Absenteeism, Stress and Health (SMASH) was a prospective cohort study among almost 1800 workers from 34 different companies with a follow-up of three years. SMASH investigated work-related risk factors for low-back, neck and shoulder pain. At baseline, localised musculoskeletal discomfort (LMD) in each body region was rated once before work and six more times during a working day. Questionnaires were sent out at baseline and three times annually during follow-up. In these questionnaires, workers were asked whether they had had low-back, neck or shoulder pain in the past 12 months, using an adapted Dutch version of the Nordic Questionnaire (Kuorinka et al. 1987). An incident case of low-back, neck or shoulder pain was defined if a pain-free episode (no or sometimes pain in the past 12 months) was followed by an episode with pain (regular or prolonged pain in the past 12 months). 2.2 SubjectsA study population was selected based on the following inclusion criteria. First, workers had to complete the baseline questionnaire; 1789 (87%) of the 2064 workers who were invited to participate in SMASH did so. Furthermore, workers had to work at least one year in their current job for more than 20 h per week and should not receive a sickness benefit or a permanent disability pension (n = 1578). Furthermore, data on LMD of the low-back, neck or shoulder region should be available (n = 1420). Finally, workers had to report no or sometimes pain in the 12 months previous to the baseline measurement (n = 913, n = 1055, n = 1146, n = 1181 for low-back, neck, right and left shoulder pain, respectively), and the question on musculoskeletal pain had to be answered in at least one follow-up questionnaire. This resulted in a dataset of 865, 1001 and 1083 and 1119 workers in the analyses of low-back, neck, right and left shoulder pain, respectively. 2.3 Localised musculoskeletal discomfortThe LMD method (van der Grinten and Smitt 1992) was based on the Borg category ratio (CR-10) scale (Borg 1990), as shown in Appendix 1. The LMD method used both numbers and verbal intensity descriptors to rate the level of discomfort. The scale ranged from 0 (no discomfort at all) to 10 (extreme discomfort, almost maximum). Except for the rating of 0.5 (extremely little discomfort), only round numbers were presented. However, workers were free to choose any intermediate number using decimals. Workers were asked to indicate their LMD ratings in 13 parts of the body using an adapted body map of the back of the body (see Figure A1), the focus being on the low-back, the neck and the right and left shoulders. During the introduction, the method was explained to and briefly tried out by the workers. At baseline, LMD was measured six times during one particular working day: 90, 50 and 10 min before lunch; just after lunch; and 40 and 80 min after lunch. In addition, one measurement was assessed before the start of the working day to have an indication of the discomfort caused by factors other than work on the measurement day. This first measurement was excluded from the analyses, because the focus of interest was discomfort caused by the activities at work. A discomfort level of 2 (little discomfort) was defined as the cut-off point for the peak discomfort measure. This level was put forward as an evaluation criterion in the International Standards Organization guideline ISO/FDIS 11226 for static working postures (International Organization for Standardization 2000), which states that a holding time-recovery scheme during work should be chosen so that discomfort would not exceed 20% of the maximal holding time during static working postures. The guideline considers that a rating of 2 on the Borg CR-10 scale is the equivalent of 20% of the maximal holding time. In the present study, workers reporting a rating of zero at each of the measurements during a working day (except for the measurement before work, which was discarded) were considered to be the reference group. The other workers were divided into a group reporting LMD ratings of 2 or lower at each of the six measurements (but at least one LMD rating higher than zero) and a group reporting LMD ratings higher than 2 for at least one of the six measurements (exceeding the guideline). With regard to cumulative discomfort measure, again the reference group consisted of the workers reporting a rating of zero at each of the six measurements during the working day. For the other workers, the sum of the six LMD ratings during the working day was calculated. To be able to find a potential dose-response relation, these workers were divided into two groups. With the lack of a recognised physiological cut-off point, the median value of the summed ratings was used to divide these workers into two equal groups. 2.4 Data analysesTo investigate the relationship between LMD at baseline and the risk of future low-back, neck or shoulder pain among symptom-free workers at each of the three follow-up times, data were analysed using Poisson generalised estimation equations (GEE). This longitudinal regression analysis technique corrects for dependency between the repeated measures of pain (Checkoway et al. 2003, Twisk 2003). Univariate and multivariate relative risks (RR) and 95% CI were estimated. In the multivariate analyses, gender and age were selected a priori as confounders, as well as follow-up time to adjust for a potential time effect. Other potential confounding factors (self-reports) were analysed separately, including years of employment, number of work hours per week, BMI, co-morbidity regarding other musculoskeletal pain at baseline and during follow-up, physical load during leisure time (Hildebrandt and Douwes 1991, van den Heuvel et al. 2005), general health status, physical activity, psychosocial factors (dimensions of the Demand-Control Support Model of Karasek et al. (1998)) and coping style (Schreurs et al. 1988). If the crude beta coefficients changed by at least 10%, the confounder was included in the final multivariate models. 3 Results3.1 Descriptive statisticsThe mean age in the study population was 35 (SD 8.7) years and 71% were men. On average, they had worked for nine years in their current job (SD 7.6) for 38 (SD 5.1) h per week; 63% had a blue-collar profession. During the three years of follow-up, 9.8% of the workers experienced an incident episode of low-back pain, 5.8% of neck pain, 5.4% of shoulder pain at the right side and 5.8% of shoulder pain at the left side. Figure 1 presents the mean LMD ratings before work and at the six measurements during the working day for the low-back and neck regions (taking the mean of left and right body sides) and for the right and left shoulders. The ratings increased during the morning, decreased after the lunch break and increased again during the afternoon until the end of the working day. The mean LMD ratings were low, due to the large percentage of the workers who reported a rating of zero at all measurements (76% for the low-back, 88% for the neck and left shoulder and 86% for the right shoulder). The standard deviations of LMD were between 0.51 and 0.78 for the low-back region, between 0.37 and 0.53 for the neck region and between 0.35 and 0.56 for the shoulder regions, respectively. 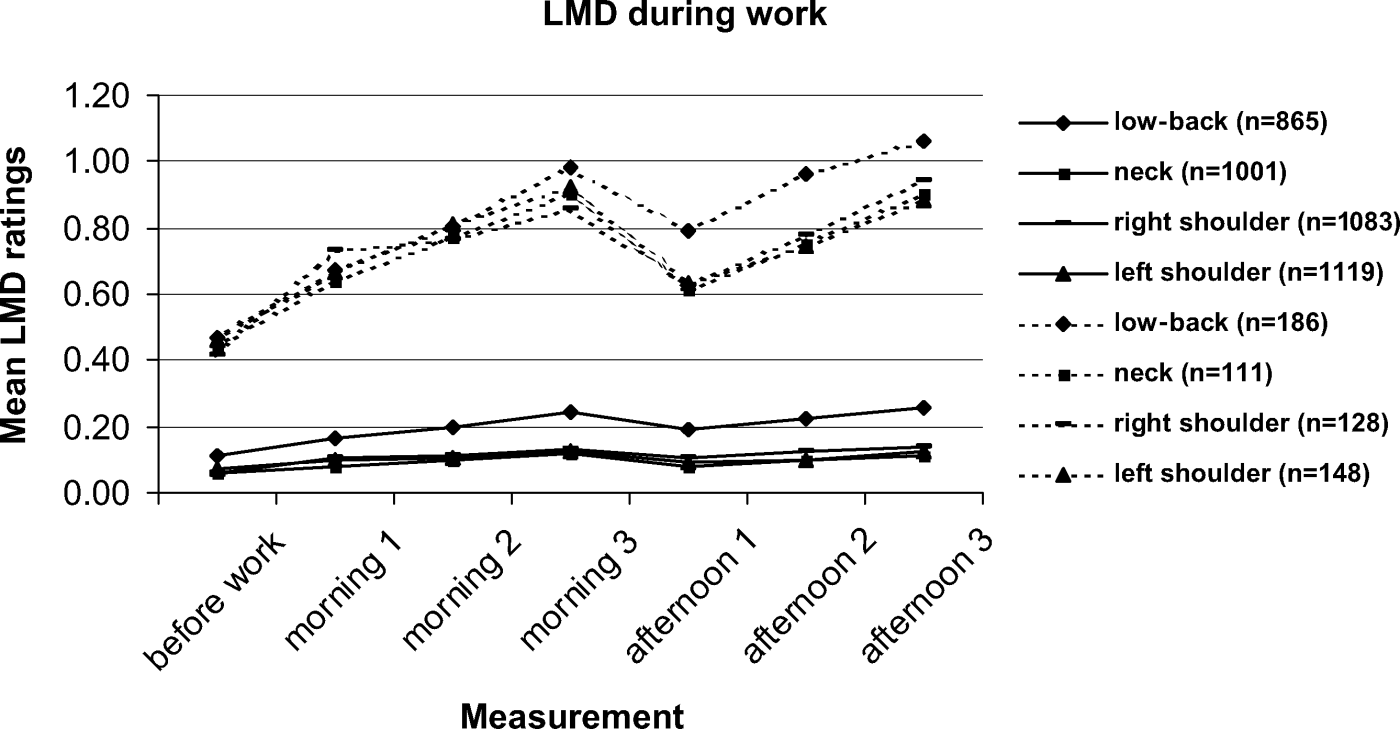 Figure 1. Mean
localised musculoskeletal discomfort (LMD) in the low-back, neck and
shoulder regions over the course of the working day. Solid lines
represent the whole study sample; dashed lines represent the group of
workers who reported LMD ratings higher than zero at least once in the
day. Figure 1. Mean
localised musculoskeletal discomfort (LMD) in the low-back, neck and
shoulder regions over the course of the working day. Solid lines
represent the whole study sample; dashed lines represent the group of
workers who reported LMD ratings higher than zero at least once in the
day.
3.2 Peak localised musculoskeletal discomfort as a predictor of future low-back, neck or shoulder painTable 1 shows the results of the univariate and multivariate GEE analyses for peak discomfort, in which the group exceeding the discomfort level of LMD rating 2 and the group with at least one LMD rating higher than zero but none exceeding 2, were compared with the reference group of those who reported a LMD rating of zero at each of the six measurements during the day.
Working exceeding the discomfort limit of 2 was found to be a predictor of future low-back pain (RR 1.79, borderline significant), neck pain (RR 2.56) and right shoulder pain (RR 1.91) but not for left shoulder pain (RR 1.90, NS). Except for right shoulder pain (RR 1.61, borderline significant), working at less than the discomfort limit of 2 did not predict pain compared to the reference group. 3.3 Cumulative localised musculoskeletal discomfort as a predictor of future low-back, neck or shoulder painTable 2 presents the results related to cumulative discomfort. Compared to the reference group, the group of workers reporting the highest LMD ratings (>3.0) had an increased risk of neck and right shoulder pain (RR 2.35 for neck pain, RR 2.45 for right shoulder pain) but not of low-back pain or left shoulder pain (RR 1.32 and 1.63, NS). No relationship was found for the group of workers who reported low LMD ratings (0-2).
4 Discussion4.1 Main resultsThe aim of this study was to investigate whether high levels of musculoskeletal discomfort and/or cumulative discomfort were predictors of future low-back, neck or shoulder pain among symptom-free workers. The discomfort limit in the ISO/FDIS 11226 guideline was used to determine a cut-off of peak discomfort. In this study, it was found that peak discomfort was a predictor of future low-back, neck and shoulder pain and that cumulative discomfort was a predictor of future neck and shoulder pain. 4.2 Comparisons with former researchTo the authors' knowledge, the relationship between musculoskeletal discomfort and future musculoskeletal pain among symptom-free subjects has been studied previously in only one longitudinal study (Werner et al. 2005a,b), which found that, in a cohort of 501 industrial or clerical workers, baseline neck or shoulder discomfort significantly increased the risk of becoming an incident case of upper extremity tendonitis during 5.4 years of follow-up on average (odds ratio (OR) 1.84 (95% CI 1.03-3.29)). Furthermore, for the worst regional discomfort rating (on a 0-10 rating scale) from any upper extremity region at baseline, the risk of future tendonitis significantly increased for every 1 point increase (OR 1.21 (1.06-2.38)) (Werner et al. 2005b). These results cannot be compared directly with the results of the present study, due to different outcome measures, but there seem to be similarities between the results for neck and shoulder pain and those of Werner et al. (2005b) regarding upper extremity tendonitis. Since it was hypothesised that peak and cumulative discomfort are indicators of biomechanical peak or cumulative exposure, respectively, the biomechanical literature reporting on peak or cumulative workload in relation to musculoskeletal pain can be used as a background. From biomechanical studies, there is evidence that both peak spinal loading (Norman et al. 1998, Kumar 2001, Village et al. 2005) and cumulative spinal loading (Kumar 1990, 2001, Norman et al. 1998, Seidler et al. 2001, Village et al. 2005) can contribute to the development of low-back pain. The present study found an association with low-back pain only for peak discomfort and not for cumulative discomfort. Furthermore, it is well known that some psychosocial factors at work are assumed to be risk factors for musculoskeletal pain (Bongers et al. 2006). Referring to the hypothesis that musculoskeletal discomfort is a predictor for musculoskeletal pain, it is convincing that musculoskeletal discomfort could be an indicator of psychosocial exposure as well. However, only one study could be found reporting on this relationship (Bystrom et al. 2004). In this study, physical discomfort (on a scale between 0 and 6) was found to be a mediating factor in the relationship between psychological workload and musculoskeletal pain. 4.3 Strengths and weaknesses of the studyStrengths of the present study were the large study population and the prospective cohort study design with a follow-up time of three years. Self-reports of musculoskeletal pain were assessed three times annually during follow-up. The test-retest reliability of the LMD method was acceptable, both for static workloads (correlation coefficient: back-neck region 0.73; shoulder-arm region 0.74) (van der Grinten 1991) and in more dynamic types of work (correlation coefficient: back-neck region 0.71; shoulder-arm region 0.78). The study contained data on fluctuations of musculoskeletal discomfort during a working day, because it was recorded three times in the morning and three times in the afternoon. However, this study had some weaknesses as well. First, it is debatable to what extent the concept of discomfort differs from the concept of musculoskeletal pain, resulting in the question as to what extent discomfort can predict pain. However, it is thought that the concepts differ, because discomfort is measured as a short-term effect of an imbalance between physical capacity and exposure to work-related physical factors (i.e. the amount of discomfort on one particular working day) and pain is measured as a long-term effect (i.e. regular or prolonged pain in the past 12 months). Furthermore, a pain-free population at baseline was chosen to avoid any distortion of the measurements of discomfort due to pain. However, the risk of misclassification cannot be totally excluded. Therefore, the conclusions have to be interpreted with caution. Second, for peak discomfort, the cut-off based on the ISO/FDIS 11226 guideline (International Organization for Standardization 2000) was considered appropriate, since work exceeding the discomfort limit of 2 is a risk factor for low-back, neck and shoulder pain. However, the guideline states that musculoskeletal discomfort may exceed the rating of 2 only if it will be followed by a recovery time, such that the remaining endurance capacity is not below 80%. From that perspective, the chosen cut-off in this study can be seen as too strict, which could have led to an underestimation of effects. Third, for cumulative discomfort, it was difficult to indicate a cut-off of the sum of LMD ratings, above which the risk of future musculoskeletal pain would increase considerably, because the distribution of LMD ratings was skewed to the right in this dataset. A large proportion of workers reported a rating of zero at each measurement and, for the other workers, the sum of the six LMD ratings was also low. This led to a median sum of LMD rating around 3. In additional analyses using different cut-offs, ranging between sum scores of 0.5 and 18, a dose-response relationship was found for shoulder pain, with an increase in effect for higher cut-offs. However, this was not found for low-back and neck pain. Finally, in spite of the selection of workers who reported no or sometimes low-back, neck or shoulder pain in the past 12 months, the results could have been influenced by the workers who reported sometimes pain. In additional analyses, it was found that reporting sometimes pain was a confounder in the relationships studied, leading to lower risk ratios. Furthermore, since musculoskeletal pain recurs frequently, these workers could have had pain earlier in the past. In this dataset, 37% of the population had experienced previous low-back or neck pain and 60% of the population had experienced previous shoulder pain in the past. In studies reported in the literature, a previous episode with pain has been found to be an important risk factor of experiencing pain again in the future (de Vet et al. 2002, van Tulder et al. 2002). In additional analyses, it was found that reporting previous low-back, neck or shoulder pain in the past ('yes' or 'no') was a confounder, leading to lower risk ratios. Nevertheless, it was decided not to adjust for these two confounders in the presented analyses because this would have led to an over-correction of the results, due to the recurrent character of musculoskeletal pain (de Vet et al. 2002). It was assumed that correction for sometimes pain in the past 12 months or correction for previous pain would lead to results for a very healthy working population. The workers in this dataset were considered to be 'normal' workers. 4.4 Ergonomic implications of localised musculoskeletal discomfortMeasurements of musculoskeletal discomfort are often used to indicate short-term effects of ergonomic interventions (Genaidy et al. 1995, Galinsky et al. 2000, Mclean et al. 2001, Fenety and Walker 2002, Babski-Reeves et al. 2005). From the results of the present study, it can be concluded that peak or cumulative discomfort, measured at several times during a working day, can also be used as a predictor of future pain among healthy workers. Even relatively low ratings can yield an increased risk of future low-back, neck and shoulder pain compared to reporting a rating of zero at each of the measurements. However, in the mixed working population of the SMASH study, only the low region of the Borg CR-10 scale was used. When stratified for the type of work, the sums of LMD ratings of the low-back and shoulder regions appeared to be only a little higher among blue-collar workers compared to white-collar workers. For the neck region, the sum of LMD ratings was only a little higher among white-collar workers compared to blue-collar workers. If the LMD method is to be used as a predictive screening instrument, many workers should be tested to find only a few with an increased risk of developing musculoskeletal pain. It is questionable if a 10-point scale is appropriate to measure musculoskeletal discomfort among healthy workers in ergonomically well-designed workplaces. Perhaps, a smaller detectable scale should be used to obtain more sensitive measures of discomfort or it might be better to apply the LMD method selectively among high-risk-workers (Lotters et al. 2003). More research is needed to investigate this. 5 ConclusionThe results of this study verified the hypothesis that high levels of musculoskeletal discomfort and/or cumulative discomfort among symptom-free workers may develop into musculoskeletal pain in the long term. The results of the study suggest that both peak and cumulative discomfort could predict future musculoskeletal pain. Appendix 1: Measurement of localised musculoskeletal discomfortA short explanation of the localised musculoskeletal discomfort (LMD) method during the field studies gave the following explanation:
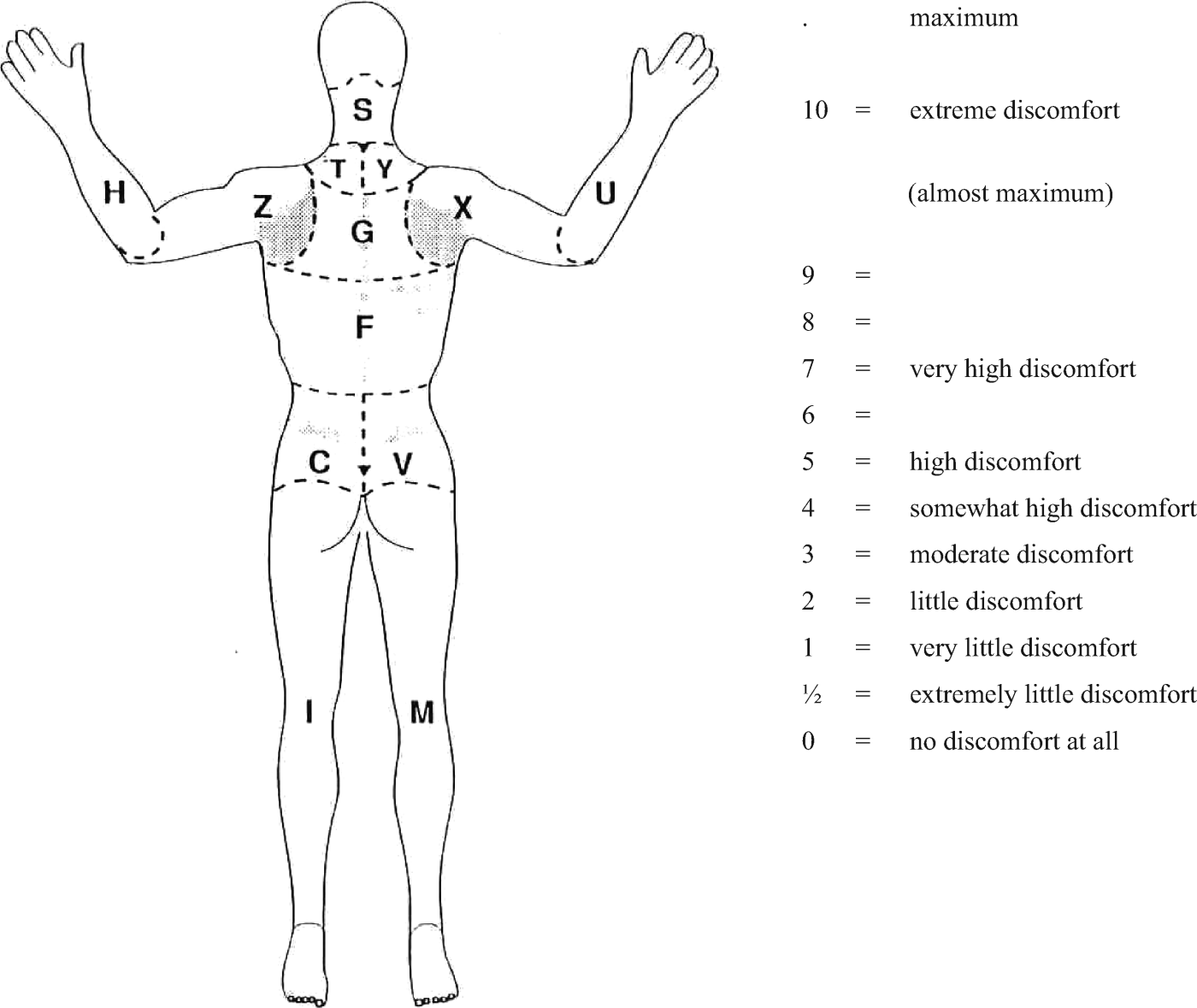 Figure A1. Adapted body map used to measure localised musculoskeletal discomfort. Figure A1. Adapted body map used to measure localised musculoskeletal discomfort.
References
List of Figures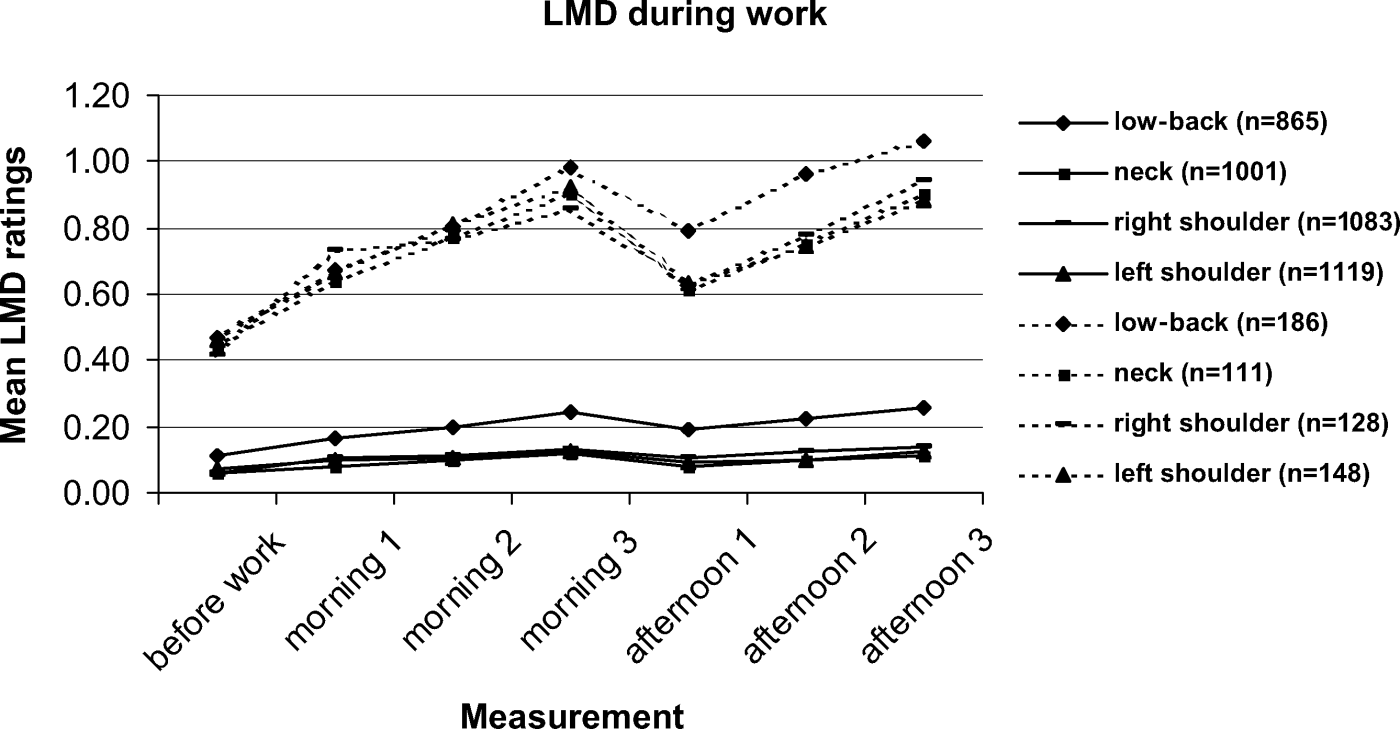 Figure 1. Mean
localised musculoskeletal discomfort (LMD) in the low-back, neck and
shoulder regions over the course of the working day. Solid lines
represent the whole study sample; dashed lines represent the group of
workers who reported LMD ratings higher than zero at least once in the
day. Figure 1. Mean
localised musculoskeletal discomfort (LMD) in the low-back, neck and
shoulder regions over the course of the working day. Solid lines
represent the whole study sample; dashed lines represent the group of
workers who reported LMD ratings higher than zero at least once in the
day. 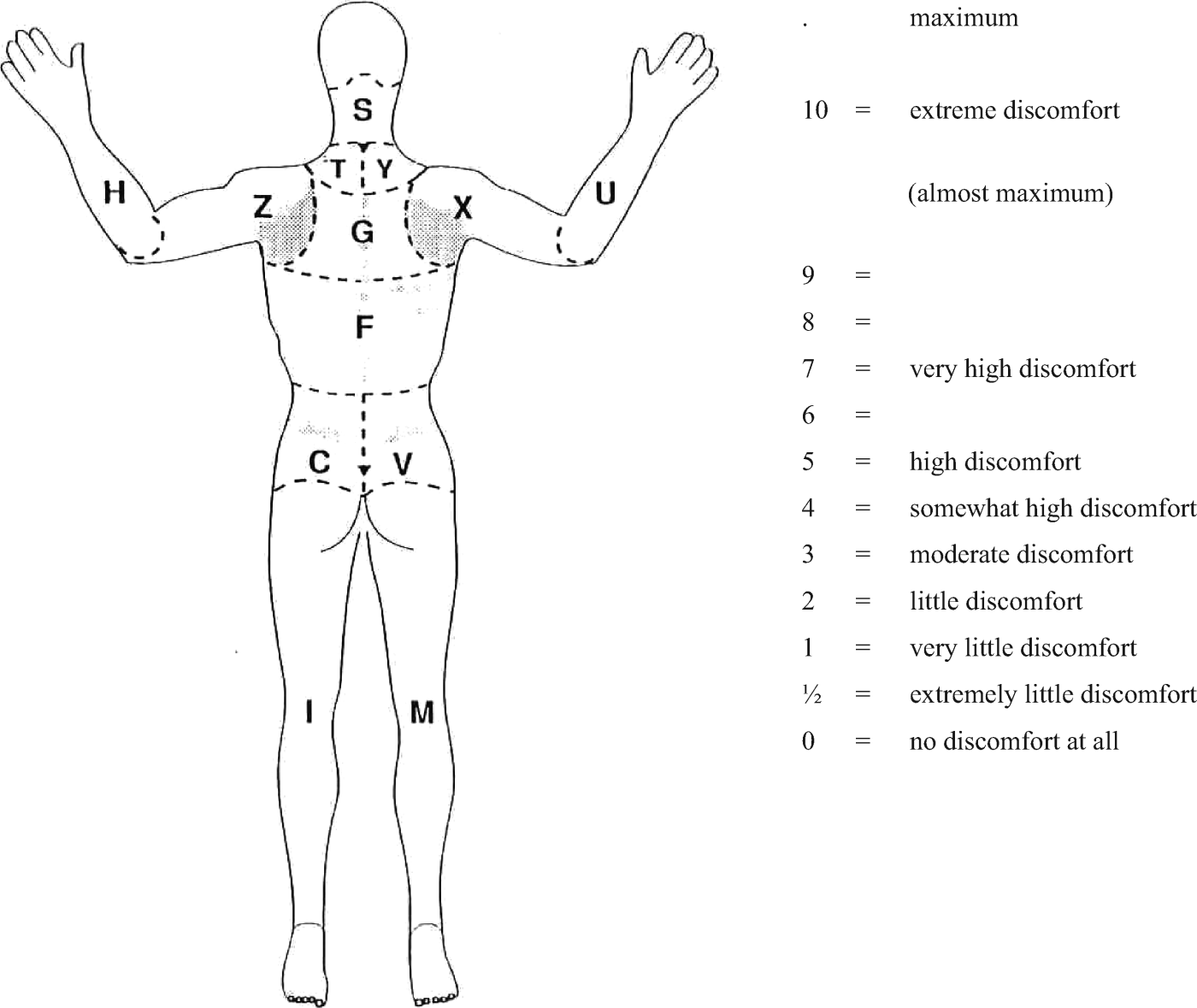 Figure A1. Adapted body map used to measure localised musculoskeletal discomfort. Figure A1. Adapted body map used to measure localised musculoskeletal discomfort. List of Tables
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Privacy Policy | Terms & Conditions | Accessibility | RSS |
|
FAQs in: English . Français . Español . 中文(简体和繁體)
© 2010 Informa plc |